Here is a story that was presented online. This woman had profolactic double mastectomy because she had the BRAC-1 genetic predisposition (much like Angelina Jolie). However, every surgeon and plastic surgeon is different.
I also had a bi-lateral mastectomy, but my scars are only on the side, and we did perform the nipple-sparing techniques after testing the nipple tissue and determining it was free of cancer. Had I not done so, the techniques used these days are actually tattoos of nipples which look similar.
I too do not regret my choices, and especially my choice of surgeon and plastic surgeon, and no, I don’t hide my body. I wear my scars like my breast cancer necklace. My warrior trophy… afterall, I’m still here and enjoying life.
Here’s another woman’s story:
“Before my surgery, I spoke openly about my decision to undergo a prophylactic bi-lateral mastectomy in the wake of a BRCA-1 diagnosis. I’m now about six weeks post-surgery, the (proud?) owner of two brand spanking new “foobs” (fake boobs), and I’ve had some time to process the new additions.
First, I believe there’s a huge misconception among the general populous about what it means to have one’s breasts removed and replaced with artificial ones (if they are replaced at all). When speaking about my upcoming surgery, I had many well-meaning people say things like, “Well at least you get new boobs!” and, “Your husband must be so excited… has he picked ’em out yet?”
Yeah, well, it’s not quite like that. Not at all, in fact.
It seems that those not in the know tend to equate post-mastectomy reconstructed breasts with augmented breasts or “boob jobs.” Nothing could be further from the truth. You see, augmented breasts are actually real live breasts with nipples and healthy breast tissue behind which silicone or saline implants have been placed, either under or above the muscle, thereby pushing them up and out. We all know what augmented breasts look like; some of them look very real, and many of them look stunningly beautiful. If augmented breasts didn’t look damn good, breast augmentation surgeries would not be so, ahem, popular.
So even though augmented boobs are often called “fake boobs,” they’re really not. I, on the other hand, do have fake boobs (or “foobs,” as I have become prone to calling them).
What is attached to my chest right now are a pair of silicone implants with no breast tissue in front of them. I am essentially sporting implants covered with skin. There are no real breasts there to hide the fact that my “breasts” are just implants — man-made, silicone-filled implants which feel like gel-filled bags and ripple when I move certain ways.
And right now, I have no nipples either. Because leaving enough breast tissue behind the nipple to spare it can create more risk, in that cancer can still occur in the tissue left behind. Also, if the surgeon failed to leave enough tissue attached to the nipple, the nipple could become necrotic and die. As in, turn black and fall off.
No thank you. I wasn’t that attached to my nipples.
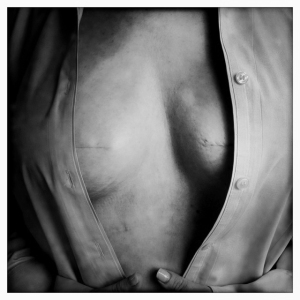
So I opted against nipple-sparing surgery, and currently have long incisions where my nipples used to be. To put it graphically — but not so graphically that it would require a “warning” tag when published — I went from looking like this:

To looking like this:
 (Hopefully you get the idea, despite my crude pencil sketches.)
(Hopefully you get the idea, despite my crude pencil sketches.)
And the view from above right now is even weirder for me. I went from seeing this:
 To this:
To this:
 Now, don’t get me wrong. I have no regrets about my decision to have preventative surgery. None, whatsoever. I sleep better knowing that I just shaved about 77 percent off of my 87 percent risk of contracting breast cancer in my lifetime. Nor am I unhappy with my results. I had excellent surgeons and my reconstructed breasts look just like they’re supposed to look at this stage. I will have skin-grafted, man-made nipples attached in the next few months, and later have color tattooed on them for good measure. The new nipples (“fips”) will hide some of the existing scars, and hopefully will be nice and round and perky. But they’ll have no feeling. They’ll just be there as accessories. Like earrings.
Now, don’t get me wrong. I have no regrets about my decision to have preventative surgery. None, whatsoever. I sleep better knowing that I just shaved about 77 percent off of my 87 percent risk of contracting breast cancer in my lifetime. Nor am I unhappy with my results. I had excellent surgeons and my reconstructed breasts look just like they’re supposed to look at this stage. I will have skin-grafted, man-made nipples attached in the next few months, and later have color tattooed on them for good measure. The new nipples (“fips”) will hide some of the existing scars, and hopefully will be nice and round and perky. But they’ll have no feeling. They’ll just be there as accessories. Like earrings.
And while I still look cute in a sexy bra, I no longer walk around topless, and now tend to sleep in camisoles rather than in the buff. I’m also somewhat shy around my husband, and am still shocked at times when I look in the mirror. It’s an adjustment, for all of us, even my toddler who gently pats the boo-boos she now sees on my chest.
For me, the psychological impact of losing my breasts was much greater than the physical impact. I am healing rapidly and know that the physical scars will fade. I also know that I made the right decision for me and my family. But those of us who either opted to have mastectomies as a preventative measure, or had mastectomies as a life-saving measure, aren’t excited about our “new boobs.” In truth, we’ll never be the same. We see ourselves differently now when we look in the mirror, because we are different, inside as well as outside.
But at least we’re here, stronger and wiser for the experience.”


 Interesting new technique. Here’s my concern…. when I was diagnosed with DCIS (ductal carcinoma in Situ), they identified one area. Post mastectomy and upon analysis of the tissue removed, they found other DCIS cells not previously identified.
Interesting new technique. Here’s my concern…. when I was diagnosed with DCIS (ductal carcinoma in Situ), they identified one area. Post mastectomy and upon analysis of the tissue removed, they found other DCIS cells not previously identified.

 “Researchers say they’ve developed a blood test that can detect some cases of early stage lung and prostate cancer.
“Researchers say they’ve developed a blood test that can detect some cases of early stage lung and prostate cancer.
 Ladies… are you taking vitamin D supplements to assist with calcium absorption to prevent osteoporosis? Well, so am I… and guess what a new study reveals – Higher levels of vitamin D, still within the normal range, are associated with an increased risk of non-melanoma skin cancer.
Ladies… are you taking vitamin D supplements to assist with calcium absorption to prevent osteoporosis? Well, so am I… and guess what a new study reveals – Higher levels of vitamin D, still within the normal range, are associated with an increased risk of non-melanoma skin cancer.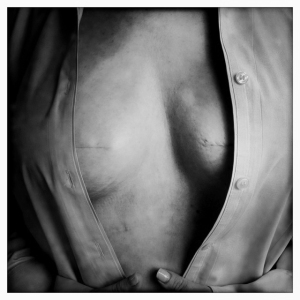

 (Hopefully you get the idea, despite my crude pencil sketches.)
(Hopefully you get the idea, despite my crude pencil sketches.) To this:
To this: Now, don’t get me wrong. I have no regrets about my decision to have preventative surgery. None, whatsoever. I sleep better knowing that I just shaved about 77 percent off of my 87 percent risk of contracting breast cancer in my lifetime. Nor am I unhappy with my results. I had excellent surgeons and my reconstructed breasts look just like they’re supposed to look at this stage. I will have skin-grafted, man-made nipples attached in the next few months, and later have color tattooed on them for good measure. The new nipples (“fips”) will hide some of the existing scars, and hopefully will be nice and round and perky. But they’ll have no feeling. They’ll just be there as accessories. Like earrings.
Now, don’t get me wrong. I have no regrets about my decision to have preventative surgery. None, whatsoever. I sleep better knowing that I just shaved about 77 percent off of my 87 percent risk of contracting breast cancer in my lifetime. Nor am I unhappy with my results. I had excellent surgeons and my reconstructed breasts look just like they’re supposed to look at this stage. I will have skin-grafted, man-made nipples attached in the next few months, and later have color tattooed on them for good measure. The new nipples (“fips”) will hide some of the existing scars, and hopefully will be nice and round and perky. But they’ll have no feeling. They’ll just be there as accessories. Like earrings.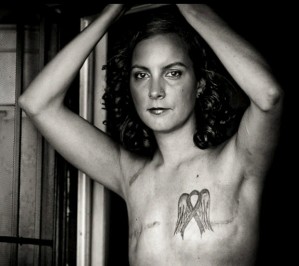 By now, most everyone has seen some of these startling and poignant photos…if you have not, please
By now, most everyone has seen some of these startling and poignant photos…if you have not, please